If you’ve ever spent the day curled up on the couch, hugging a hot water bottle, then you know that your menstrual cycle can sometimes be…well, a pain.
According to the American College of Obstetricians and Gynecologists, at least half of all women who menstruate experience some amount of period pain each month. For adolescent girls and young women in particular, the prevalence rate may be as high as 90 percent.1,2
However, for some women, period pain can be severe—enough to disrupt your daily routine. While we’re often taught that suffering through period cramps is just a part of life, the reality is that consistently severe pain can be a sign of an underlying condition. So, how can you tell if your cramps are “normal,” or if it’s time to talk to your doctor? Here’s what you need to know.

What Causes Period Pain?
Before we get into period pain severity and what’s considered “normal,” let’s get a better understanding of why we experience cramps in the first place. Dysmenorrhea—the official term for cramps and pelvic pain during your period—is most likely caused by hormone-like compounds in the body called prostaglandins. Prostaglandins are involved in a variety of bodily processes, including blood flow, healing and inflammation. They’re also responsible for the uterine contractions that help your body shed the endometrium during menstruation—aka menstrual cramps, which can range from mild to severe.3,4
Research suggests women with higher levels of prostaglandins during the first two days of their period report more period pain. Up to 20 percent of women experience severe cramps—the kind that cause you to skip work or cancel plans.5,6
If you’re experiencing menstrual cramps or period pain without the presence of an underlying condition, this is called primary dysmenorrhea. But certain conditions, like endometriosis, fibroids, or pelvic inflammatory disease, can make period pain worse. If you’re experiencing unbearable period pain, it may be a sign that an underlying condition is to blame. This is known as secondary dysmenorrhea.
Understanding the difference between these two types of period pain can help you get an accurate diagnosis and find the most effective treatment options.
Primary Dysmenorrhea vs. Secondary Dysmenorrhea
Primary dysmenorrhea is period pain without pelvic pathology — in other words, the pain is caused by uterine contractions during menstruation, without any underlying condition making it worse.
“Primary dysmenorrhea refers to the crampy pain with the initiation of the first mense and continues throughout life,” says Dr. Kecia Gaither, MD, MPH, FACOG, Director of Perinatal Services and Director of Maternal Fetal Medicine at NYC Health + Hospitals Lincoln in the Bronx. “The pain reflects uterine contractions.”
This type of period pain typically starts one to three days before your period and may last for a few days. Pain from primary dysmenorrhea may be mild, moderate, or severe. Along with the achy cramps in your lower abdomen, you may also experience additional symptoms like nausea, fatigue, headache, or gastrointestinal issues like bloating or diarrhea—which can also exacerbate you’re feeling. (For what it’s worth, many doctors and women liken menstrual cramps to early labor contractions—so let’s just say that if you’re struggling, your pain is valid.)7
Secondary dysmenorrhea, on the other hand, refers to period pain that’s exacerbated by an underlying physical condition. “Underlying conditions such as uterine myomas, endometriosis, polyps (uterine growths), or adenomyosis can contribute to excessively painful periods,” Dr. Gaither says.
Secondary dysmenorrhea tends to last longer each month than normal cramps, and the pain may worsen over time. If your pain is severe or you suspect that you may be experiencing secondary dysmenorrhea, your doctor can help you identify the underlying issue and discuss treatment options.
When to Talk to a Doctor About Period Pain
Because menstrual cramps are so common, you may feel obligated to tough it out each month. It’s just part of the package deal of having a period, right? Nope. If period pain is interfering with your life, your work schedule, or your overall wellbeing, your doctor can help you get to the root of it—so that you can get some much-needed relief.
“Any cramping that is not well-controlled and impacts quality of life should be discussed with a care provider,” reiterates Dr. Caitlin O’Connor, a naturopathic doctor and midwife.
Another sign that it’s time to talk to your doctor: Your cramps don’t respond to the usual remedies such as over-the-counter pain relievers, heating pads, light exercise, or a warm bath. This can clue you in that your period pain may be caused by an underlying condition.
Last but not least, if your period tends to affect other aspects of your health, let your doctor know. Dr. Gaither recommends telling your doctor if your period is accompanied by any of the following symptoms:
-
Anemia
-
Pain while urinating
-
Pain during bowel movements
-
Pain during sex
-
Pelvic pain
-
Back pain
Your doctor can evaluate your medical history, conduct a physical and pelvic exam, and perform imaging tests to help identify the cause and recommend the best treatment plan.8
How to Stop Period Pain at Home
For primary dysmenorrhea, there are a few simple steps you can take to help minimize menstrual cramps.
“Ginger capsules, magnesium phosphorus cell salts, heat, and gentle movement are my go-tos,” Dr. O’Connor says. “For prevention, a Mediterranean-type diet that’s high in omega-3s—along with regular exercise and supplementation with calcium and magnesium—can be really helpful.”
Research suggests certain vitamin deficiencies may be associated with severity of menstrual pain. Eating a balanced diet and supplementing with a daily multivitamin can help to ensure your body is getting the nutrients it needs each day.9
The American College of Obstetricians and Gynecology notes that over-the-counter pain relievers (ie ibuprofen) and certain types of hormonal birth control may also reduce the severity of cramps if they’re interfering with your life. A warm bath, heating pad, or hot water bottle can help to soothe an achy abdomen or lower back.
Also remember that your period isn’t your entire cycle—it’s just one part of it, and supporting your hormones throughout your menstrual cycle can correlate with your PMS symptoms. Aim to eat a balanced diet and get regular exercise throughout the month, and practice good sleep habits. During your luteal phase (the two weeks leading up to your period), take special care to treat your body gently and prioritize rest.10
But if these self-care strategies aren’t giving you enough relief, or you’re dealing with unbearable period pain, schedule an appointment with your healthcare provider. Getting evaluated can be the first step on the road to less painful periods.
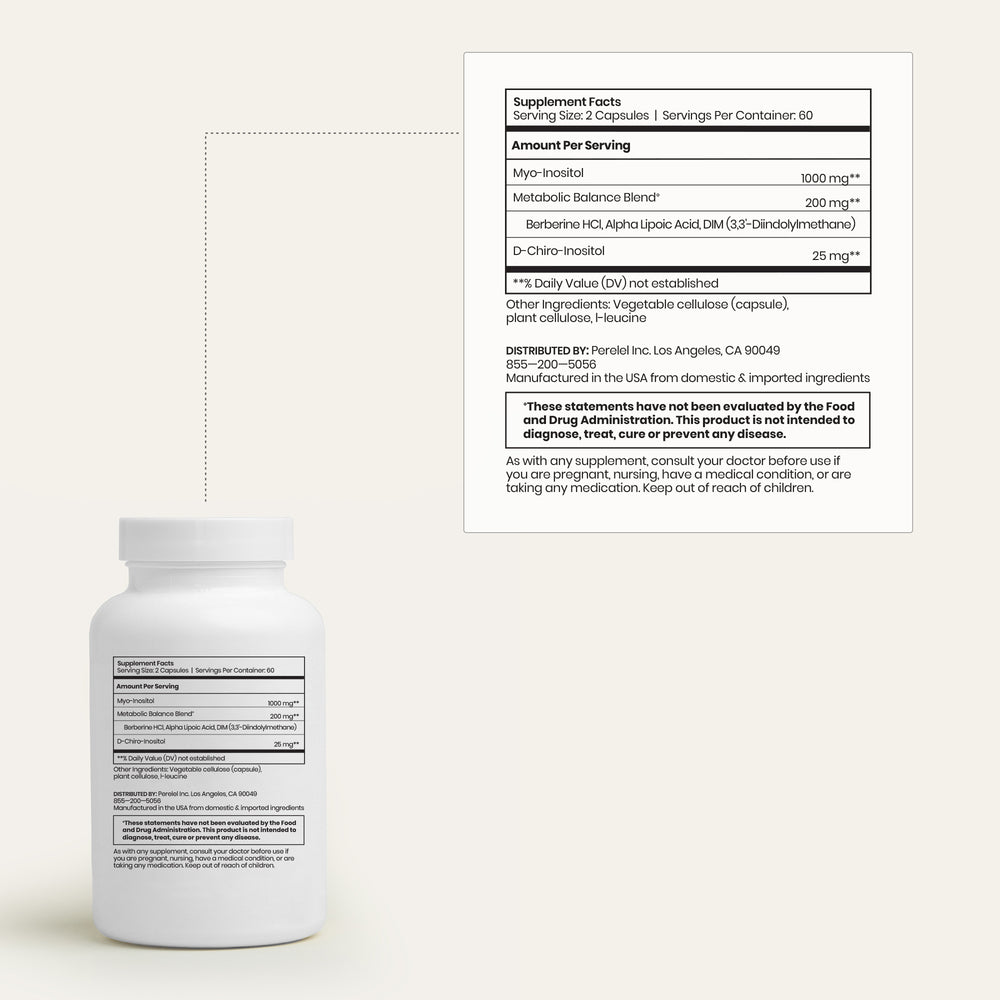
Shop the Article:
Want to go deeper on your cycle? Learn about how your body changes through each of the four phases—and how to adjust your routine accordingly.
Resources:
1 The American College of Obstetricians and Gynecologists; Dysmenorrhea: Painful Periods
3 Rania Itani et al; Primary Dysmenorrhea: Pathophysiology, Diagnosis, and Treatment Updates; Mar 2022
4 Cleveland Clinic: Prostaglandins
5 Mariagiulia et al; Dysmenorrhea and related disorders; Sep 2017
6 Hong Ju et al; The Prevalence and Risk Factors of Dysmenorrhea; Nov 2013
8 Johns Hopkins Medicine: Dysmenorhhea
10 The American College of Obstetricians and Gynecologists; Dysmenorrhea: Painful Periods