Mood swings. Appetite changes. Bloating. Fatigue. Let’s be real—when our period is coming, we can feel it. And just like the symptoms vary from person to person, so too do our coping mechanisms: Some of us white knuckle our way through the discomfort, while others pop an ibuprofen at the first sign of a headache. But while our individual responses run the gamut, one thing remains constant throughout all of our experiences: a desire for relief.
The good news? There are plenty of actions you can take to help those telltale period signs, also known as premenstrual syndrome (PMS), feel a little bit more manageable. Read on to learn about PMS, what causes it, and most importantly—how to deal with your most disruptive symptoms.
First things first: What, exactly, is PMS?
“PMS is broadly defined as changes in mood and/or physical symptoms that occur in relation to the menstrual cycle,” explains Dr. Caitlin O’Connor, a naturopathic doctor who specializes in hormonal health. Most often experienced in the one to two weeks leading up to your period (also known as your luteal phase), PMS symptoms are common, with as many as three out of every four menstruating women having experienced it in some form. In other words: You’re definitely not alone.
What are the common symptoms of PMS?
Before exploring the signs, it’s important to clear up a misconception: Contrary to popular belief, PMS doesn’t refer to what you feel during your actual period. According to Dr. Banafsheh Bayati, Perelel’s medical co-founder and a leading OB/GYN, PMS refers to the predictable, recurring symptoms that occur before your period starts. Translation? Your PMS symptoms should actually start to lessen soon after the bleeding begins.
As for symptoms, there are many—ranging from emotional to physical:
Emotional symptoms:
- Crying spells
- Mood changes
- Irritability
- Anxiety
- Depression
- Anger
- Social withdrawal
- Poor concentration
Physical symptoms:
- Bloating
- Food cravings
- Fatigue
- Joint or muscle pain
- Breast tenderness
- Insomnia
- Change in libido
- Migraines
- Acne
- Constipation or diarrhea
- Weight gain from fluid retention
As Dr. O’Connor puts it, “Almost every system can be impacted.”

How is PMS diagnosed?
Dr. O’Connor puts it simply: “There’s no specific physical exam or test that diagnoses PMS—rather, it’s a subjective assessment based on the timing of the symptoms, and the fact that they recur in a predictable pattern throughout the month.”
To better understand your PMS symptoms, your gynecologist (or health care provider) may have you track how you’re feeling in a journal or calendar for at least two periods. This will help them spot any patterns, and if necessary, prescribe any specific treatments.
What are the causes of PMS?
The exact causes of PMS have yet to be elucidated by researchers, but there are a few factors that may contribute to it.
→ Hormone levels: PMS symptoms come and go with hormonal changes, and they usually stop with pregnancy and menopause.
→ Brain chemistry: Fluctuations in a brain chemical called serotonin might trigger PMS symptoms. (Low serotonin levels can lead to mood swings, fatigue, cravings, and sleep troubles.)
→ Depression: In some cases, severe PMS is associated with undiagnosed depression—though depression itself doesn’t account for all the symptoms, something researchers are still studying.
Can PMS be treated? If so, how?
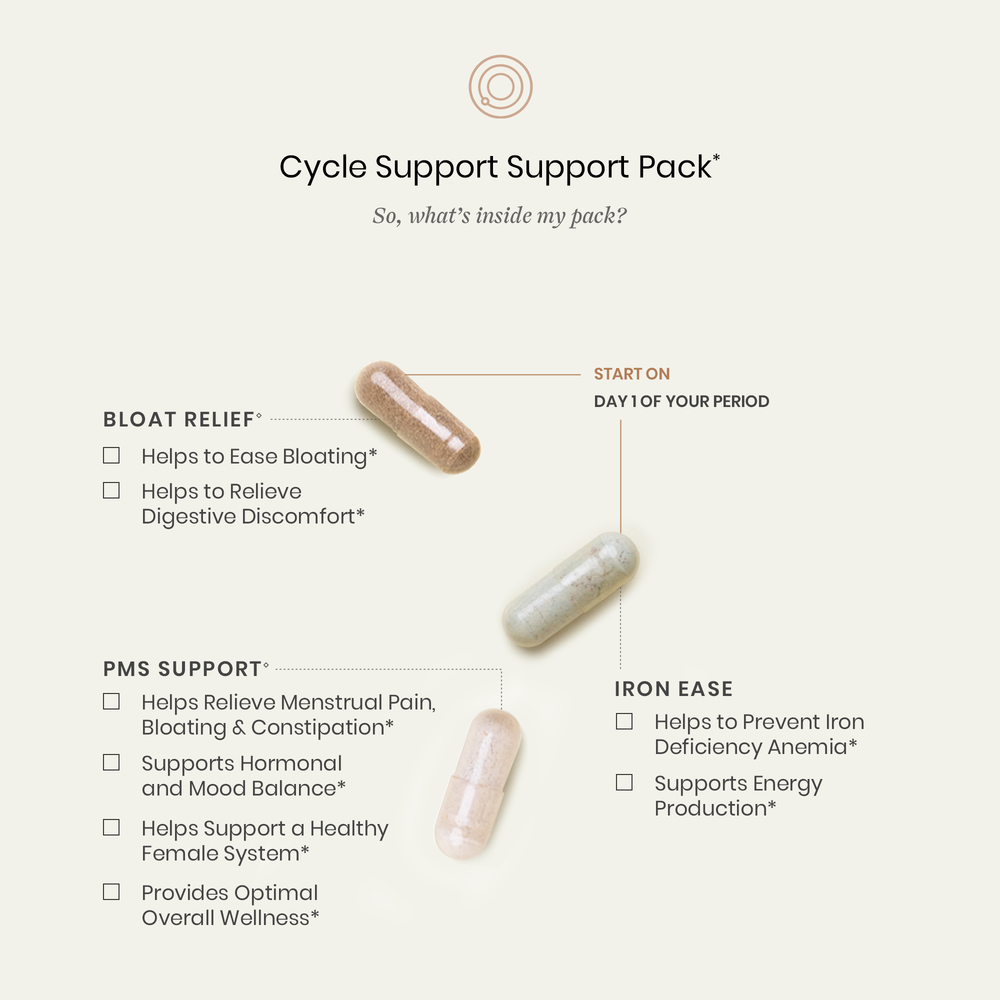
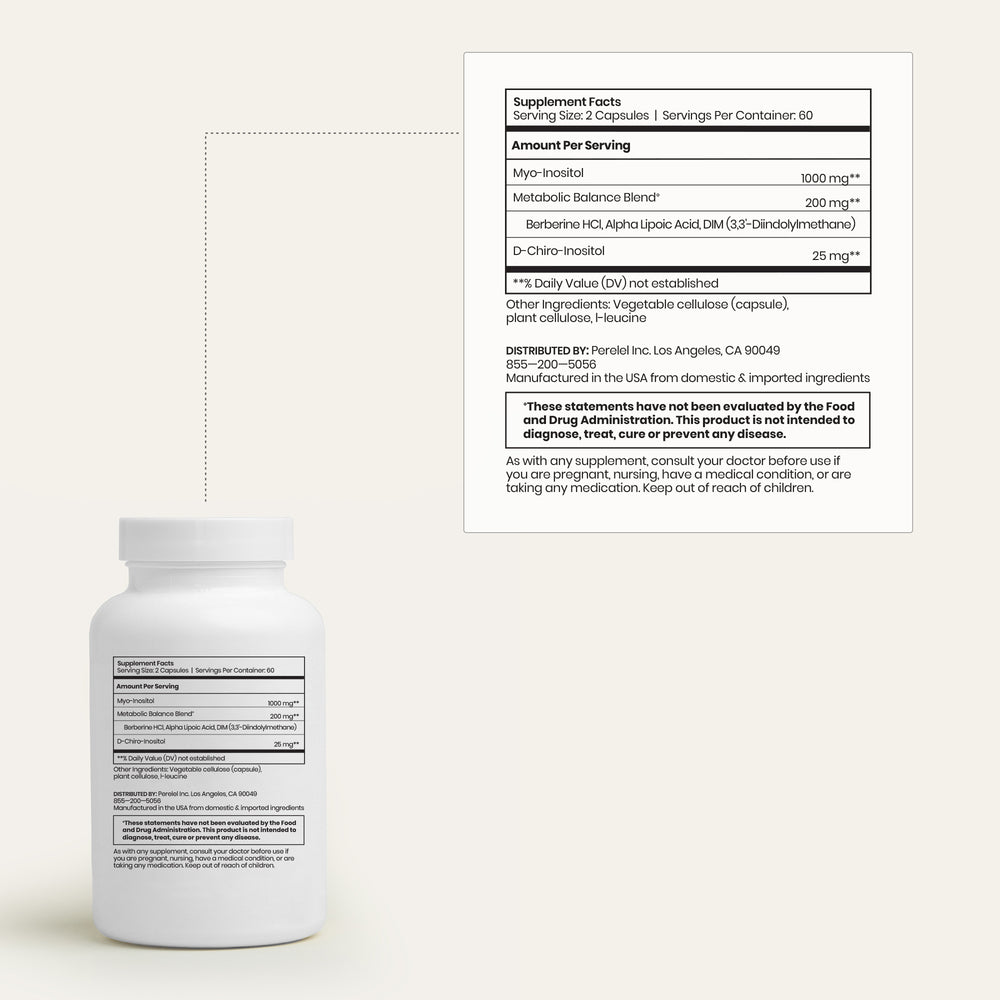
“For many women, lifestyle changes can help relieve symptoms,” says Dr. Bayati. “The success of these changes—which include dietary adjustments (reducing caffeine and alcohol intake, increasing consumption of fiber-rich whole foods); vitamin and herbal supplements (calcium, magnesium, vitamin B6, and omega supplementation have all been reported as helpful); increased cardio exercise; stress reduction; quality sleep; and alternative practices (such as acupuncture, massage, and meditation)—varies with each individual.” Dr. Bayati helped formulate our Cycle Support Pack, a vitamin pack that syncs with your menstrual cycle—targeting overall hormonal balance and symptoms like bloating, fatigue, menstrual pain, and mood swings.
Shop the Article:
She also notes that, beyond addressing PMS with your healthcare provider, the first step in managing your symptoms is practicing mindfulness in order to understand the triggers or lifestyle activities that may be exacerbating them.
Apart from the treatments mentioned above, some women will require additional assistance, whether through medications, such as non-steroidal anti-inflammatory drugs to ease the physical discomforts or selective serotonin reuptake inhibitors (SSRIs) to reduce mood symptoms. Diuretics can help with acne, excess swelling, and bloating (though Dr. Bayati prefers starting with dietary changes and gentle herbal remedies such as ginger, lemon balm, licorice root, and peppermint), while hormonal contraceptives (i.e. birth control) can be used for some tougher cases to eliminate ovulation. In other words, there are plenty of options to explore—all of which should be done in conjunction with your doctor.
What if my symptoms are particularly severe?
While the majority of women only experience a few of these PMS symptoms during their cycle, for a small number of women, the experience is debilitating enough to affect their daily lives—a severe form of PMS called premenstrual dysphoric disorder (PMDD). “PMDD can cause irritability, depression, or anxiety starting one to two weeks prior to each cycle,” says Dr. Bayati.
If you need help, seek it. Treatments exist. As Dr. O’Connor puts it: “Suffering with your cycle is certainly not optimal and does not need to be tolerated.”
We created our Cycle Support Pack with the intention of building a better relationship with our cycles—through targeted relief of symptoms like fatigue, bloating and menstrual pain, as well as promoting overall hormonal and mood balance.
Resources:
- Premenstrual syndrome (PMS). ACOG.
- Hantsoo L, Epperson CN. Premenstrual Dysphoric Disorder: Epidemiology and Treatment. Curr Psychiatry Rep. 2015 Nov;17(11):87. doi: 10.1007/s11920-015-0628-3. PMID: 26377947; PMCID: PMC4890701.
This article is for informational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and we recommend that you always consult with your healthcare provider. To the extent that this article features the advice of physicians or medical practitioners, the views expressed are the views of the cited expert and do not necessarily represent the views of Perelel.